*This web page was produced as an assignment for an undergraduate course at Davidson College*
Assignment #2: My Favorite Protein: Insulin
I. Discovery of Insulin
Diabetes was known as early as the 1st century, A.D. as a disease characterized by Arataeus as "a melting down of the flesh and limbs into urine", although the name diabetes was not yet formally attached to this disease. More understanding of how this disease functioned did not occur until the 19th century when it was found from autopsies that diabetes is accompanied by damage to the pancreas. There was much debate about the specific relationship between the pancreas and diabetes, especially between two scientists from the University of Strasbourg, Oskar Minkowski and Joseph von Mering. They disagreed about the function of pancreatic enzymes in the body, and to solve their argument, they removed the pancreas from a dog and recorded their observations. They found this dog to urinate incessantly, even when taken outside numerous times throughout the day. After testing the sugar concentration in the animal's urine, they concluded that he had become diabetic. (Research of this sort involving pancreas removal was also conducted on cats, guinea-pigs, rabbits, and rats by a variety of researchers.) Diabetic research continued into the early 1900's and at the turn of the century Eugene Opie from Johns Hopkins University discoverd that diabetes is caused by something contained within cells discovered by Hans Langerhans in 1869, now referred to as islets of Langerhans. Frederick Banting, a graduate of the University of Toronto Medical School, became interested in pancreas and diabetes research in 1920 and approached Professor John Macleod, a well-known researcher in the field of carbohydrate metabolism. Along with Charles Best, a fourth-year medical student at the time, and J.P. Collip, a well-known biochemist, these four scientists discovered a substance that when injected into a diabetic dog, abated the symptoms of diabetes. This discovery was presented in 1922 in a paper that called this substance insulin. In 1923, Banting and Macleod were awarded the Nobel Prize for their discovery of insulin. Banting shared his award with Best, and Macleod shared his award with Collip to acknowledge the invaluable contributions of these men (Bliss, 1982). The primary structure of insulin was determined in 1953 by Frederick Sanger, and despite this being an accomplishment in itself, this was also the first time that the complete amino acid sequence of a protein was determined and proved that proteins have unique covalent structures (Voet and Voet, 1995). The primary amino acid sequence of insulin is shown in Figure 1. The human insulin protein consists of two chains, A and B, which are connected via disulfide bridges. An interactive Chime tutorial about insulin can be accessed here.
Figure 1: The primary amino acid structure of human insulin. As is shown, insulin consists of two peptide chains which are connected by disulfide bonds. This figure was obtained pending permission from Dr. Harry Ungar and can be found in its original state here.
II. The Function of Insulin in the Body
Insulin is produced and secreted by ß cells within the islets of the pancreas. Figure 2 shows the large almost square-looking islets and the small circular cells within the islets of Langerhans which make and secrete insulin. Insulin is secreted into nearby blood vessels as is shown by the blue arrows and is then allowed to travel throughout the bloodstream to fulfill its function.
Figure 2: Pancreatic Islets and Pancreatic Islet Cells which produce and secrete insulin into blood vessels. This figure was reproduced pending authorization from the Norman Endocrine Surgery Clinic and can be found in its original version here.
So what is the function of insulin?
Insulin binds to a receptor on the plasma membrane of target cells, and when this insulin-receptor complex forms, glucose is allowed to enter into the target cell where it is used as an energy source or is converted into glycogen for energy storage. The insulin receptor is a protein consisting of two copies of two different peptide units, alpha and beta. One insulin molecule is required to bind to each alpha subunit, and after this occurs, the ß subunits then transmit a signal that causes the cytoplasmic end of the receptor protein to change shape. This change causes a cytoplasmic protein kinase active site to be exposed which causes the phosphorylation of an insulin receptor substrate which initiates other reactions that lead to the uptake of glucose by the cell (Purves et al, 2000). This process is shown in Figure 3.
Figure 3: Insulin-receptor complexes on the cell surface cause chemical responses to occur within the cell. This figure was reproduced pending permission from the authors of Life, 6th Ed (Purves et al, 2001).
When the concentration of glucose in the blood is high, the pancreas releases insulin into the bloodstream. The insulin travels throughout the bloodstream until it finds its receptors on the surface of cells. After two insulin molecules bind to the insulin-receptor complex, a series of complex reactions occurs which ultimately leads to the uptake of glucose by cells. These cells are then able to use glucose as an energy source. For example, fat cells use glucose to produce fat and liver cells use glucose to produce glycogen and fat to be stored for later energy use. When the concentration of glucose in the bloodstream is low, most cells in the body use glycogen and fat as their energy source instead of glucose (Purves et al, 2001).
III. Diabetes
Diabetes Mellitus is currently the 3rd leading cause of death in the United States after heart disease and cancer and affects over 135 million people worldwide. Complications from diabetes kills 2.8 million people worldwide per year. By the year 2025 over 300 million people will have diabetes (Insulin-Free World Foundation). With this disease, insulin is not produced and secreted often enough (Type 1 diabetes) or insulin receptors are not abundant enough or do not respond and initiate signals when insulin binds to it (Type 2 diabetes). Without enough insulin being produced in the pancreas or without enough insulin receptors on cells, excess glucose accumulates in the bloodstream, which causes water to move from cells into the bloodstream. The kidneys remove this excess fluid volume from the blood by increasing urine output. The cells which are supposed to receive glucose are starved and are forced to use glycogen and fat as an energy source. This causes triacylglycerol hydrolysis, fatty acid oxidation, glucoconeogenesis, and ketone body formation to be accelerated. These processes lead to a high amount of H+, Na+, K+, and water secretion in the urine, which leads to dehydration and potentially life-threatening problems (Voet and Voet, 1995). Figure 4 shows a girl with diabetes before her diabetes was treated and after she started receiving daily insulin injections.
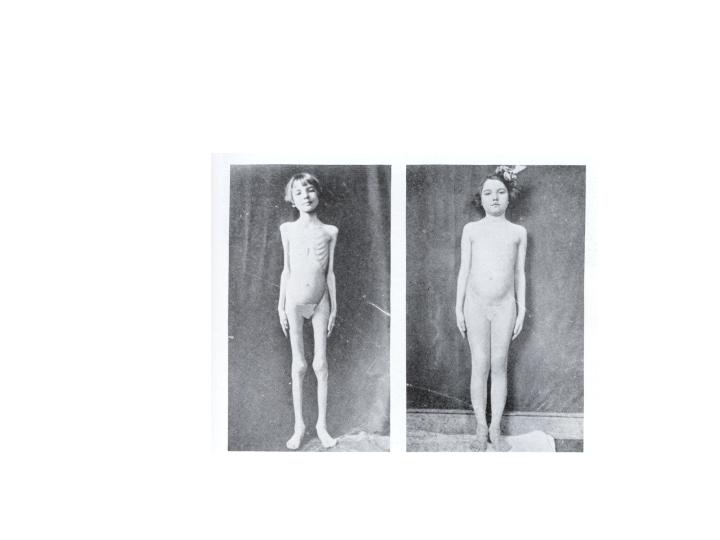
Figure 4: A girl with diabetes before all insulin treatments and after beginning treatments. These pictures were taken in 1922, soon after the discovery of insulin (Bliss, 1982).
Type 1 diabetes is the more severe form of diabetes and occurs when the pancreas lacks ß cells or has defective ß cells in the islets of the pancreas. If the pancreas lacks these cells, insulin has no chance of being produced. When these cells are present but are defective, the body thinks that these cells are foreign and it tries to kill them. Diabetes is therefore an autoimmune disorder. The mechanism for how this autoimmume reaction is not yet understood. People with Type 1 diabetes are required to supply their body with insulin via insulin shots many times a day and have to follow a very carefully balanced diet so that their glucose levels remain at a relatively constant level. This type of diabetes leads to decreased lifespans of up to 1/3 for those afflicted by it because of the degenerative complications associated with the disease. Type 1 diabetes strikes mostly children, is caused by mutations in several genes, and it is speculated that a locus on chromosome 6 harbors at least one gene responsible for diabetes susceptibility (National Center for Biotechnology Information, 2003).
Type 2 diabetes accounts for over 90% of diabetes cases worldwide and the amount of people with this form of diabetes is rapidly rising. This type of diabetes is thought to be the result of overeating. When one eats too much, too much glucose is being introduced into the body. Insulin is secreted as a response to the presence of glucose in the blood, but insulin levels are so high that insulin receptors simply cannot accomodate the amount of insulin present, and over time the receptors lose their responsiveness to insulin binding to it, or there simply aren't enough receptors to accomodate all of the insulin present in the bloodstream. This type of diabetes has historically been associated with people over the age of 40 but is increasingly being observed in children (Voet and Voet, 1995).
Diabetes is the primary cause of blindness, kidney failure, and amputation, and causes significantly shorter life expectancies for its sufferers. Currently, 1 out of 7 health care dollars is spent fighting this disease. Three different methods of curing this disease are currently available and/or are being clinically tested. One method is pancreas transplantation. More than 1300 pancreas transplantations are performed worldwide per year with an 83% success rate, but this small number of transplantations is several times smaller than the amount of diabetes sufferers in the world. One other method is Islet transplantation. Clinical trials involving this sort of transplantation hold promise as another way to make the body produce insulin. One last method that can be used to rid patients of their diabetes is to engineer human stem cells to be glucose-responsive insulin-secreting cells (Insulin-Free World Foundation).
IV: References:
Bliss, M. 1982. The Discovery of Insulin. Chicago: The University of Chicago Press.
Insulin-Free World Foundation. <http://www.insulinfree.org/factsgen.htm>. Accessed 2003 March 12.
National Center for Biotechnology Information: Genes and Disease. 2003. <http://www.ncbi.nlm.nih.gov/disease/Diabetes.html>. Accessed 2003 March 12.
Purves WK, Sadava D, Orians GH, Heller HC. 2001. Life: the Science of Biology, sixth edition. Sunderland, Massachusetts: Sinauer Associates, Inc.; p 283-284, 724, 905.
Ungar, H. 1999. <http://c4.cabrillo.cc.ca.us/projects/insulin_tutorial/tutorial/index.html>. Accessed 2003 March 12.
Voet, D and Voet JG. 1995. Biochemistry, 2nd Edition. Somerset, NJ: John Wiley and Sons, Inc.; p 106, 792-293.
Chemistry Individual Research Project, May 2002
Send comments, questions, and suggestions to cawilliford@davidson.edu