Lungs Background
Lung Physiology and
Histology
|

Image from http://www.britannica.com/EBchecked/topic-art/351473/107200/The-alveoli-and-capillaries-in-the-lungs-exchange-oxygen-for
|
Breathing and Lung Physiology
- The lung is the
location of a fast exchange of carbon dioxide for oxygen. Carbon dioxide
is a waste product of cellular respiration and is brought to the lungs
by heoglobin and escapes the body. The empty hemoglobin can then bind
oxygen carry it in the blood to all of the cells in the body.
- Diaphragm
contracts to pull on pleural membrane, allowing lungs to open
- Air
rushes through the buccal cavity, down the trachea, bronchi, and
bronchioles until it reaches the alveoli
- The
alveoli are the site of gas exchange
- There
is only a 2µM distance between the lumen of the alveoli and the red
blood cells in the capillaries
- Partial
pressure differences allow oxygen (in the alveoli) and carbon dioxide
(in the red blood cells) to exchange places via passive diffusion
(Sadava et al. 2008).
|
|
Alveolar
Histology
- Alveoli
= comprised of 2 cells: type one pneumocytes and type 2 pneumocytes
(Kathuria et al. 2007; Wang et al. 2006).
- Type
1 cells
- Comprise
95% of alveolar cells
- Site
of gas exchange
- Provide
the structural support of the alveoli
- Help
manage lung fluid homeostasis
- Little
mitotic activity
- Easily
injured
- Type
2 cells
- Approximately
5% of alveolar cells
- Mitotically
active
- Secret
and alter surfactant
- Participate
in both the immune and inflammatory responses
- Type
2 cells proliferate and transform into Type 1 cells to repair alveolar
walls; they are vital to lung function (Wang et al. 2006)
|
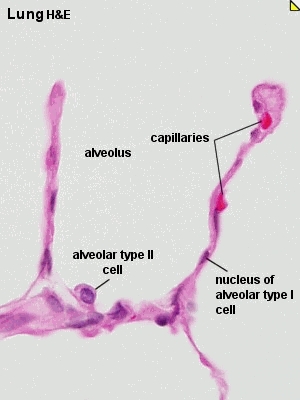
Image from http://legacy.owensboro.kctcs.edu/gcaplan/anat2/histology/histo%20F%
20respiratory%20system.htm
|
Lung Pathology
|
Lung
Defense & Pathology
Because lung cells come in contact with the air they are vulnerable to
air born pathogens (like bacteria) and antigens (like pollen). SInce they are
the first line of defense, lung cells must protect not only themselves but
also the rest of the body from airborn pathogens.
Mechanisms for protection rely on excluding the antigen or providing a barrier:
- Muco-cilliary
escalator
- Some
lung cells secrete mucous to trap bacteria and potential pathogens
- Lung
cells with specialized cilia sweep the mucous up towards the mouth
- Trapped
pathogens then exit the body when the mucous is coughed up (Sadava et
al. 2008).
- Activation
of the Innate Immune System
- The
immune system “recognizes” an antigen through structural barriers or
microbial pattern recognition sequences, then it will induce an inflammatory
response (Hollingsworth et al. 2007).
- Inflammatory
response is marked by the “respiratory burst” of activated leukocytes,
causing surrounding cells to uptake oxygen and release reactive oxidative
species (ROS) into the interstitial fluid (Chen et al. 2007; Balmes 1993).
- Uptake
of oxygen allows neighboring cells to increase mitochondrial activity
(vital for mitosis)
- Release
of ROS is an attempt to harm antigens more than the organ itself (Felty
et al. 2003).
- Results
in decreased lung function due to pulmonary edema and epithelial cell
injury (Chen et al. 2007; Balmes 1993).
Despite these defense mechanisms, certain antigens are still able to damage
the lung tissue and cause the diseases such as asthma, acute respiratory
distress syndrome (ARDS), chronic obstructive pulmonary disease (COPD) and
cancer. |
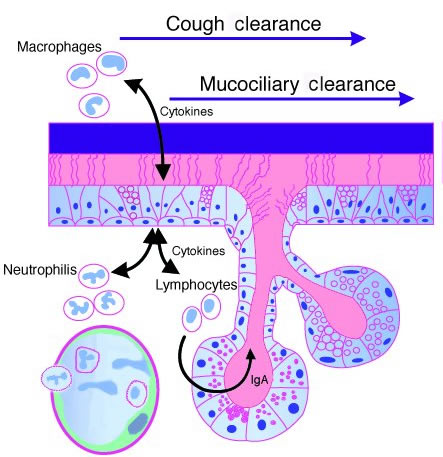
Image from http://www.jci.org/articles/view/6277/figure/1
|