Overview of Epithelial Cells
The diversity of epithelial cells makes for an interesting field of study. Our lab is dedicated to studying various aspects of rat alveolar type II (L2) lung under a variety of conditions in order to answer specific research questions. The following provides a general overview of of the six types of epithelial cells, how structure relates to function, and why research in this field is important and relevant. |
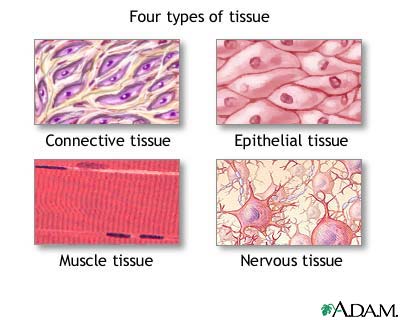 Image from: http://www.pennmedicine.org/encyclopedia/em_PrintArticle.aspx?gcid=004012&ptid=1 Figure 1.The four major tissue types in humans. |
|
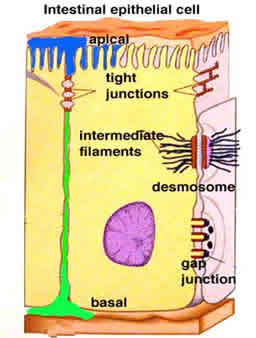 Image from:http://cellbiology.med.unsw.edu.au/units/science/lecture0808.htm Figure 2. Epithelia are apical to the basement membrane and are characterized by the presence of tight junctions. |
Avascular
Sensory
Gliding surface layer
|
Transitional
Tight barrier
Different from endothelial cells
|
Where Are Epithelial Cells Found?
- Epithelial cells line the major cavities of the body.
- Epithelia form the structure of the lung, including the alveoli or air sacs where gas exhange occurs.
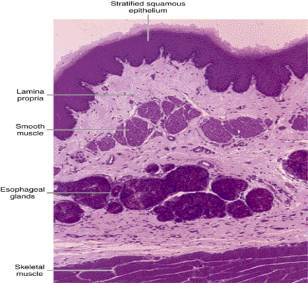
- Cells line most organs, such as the stomach and small intestine, kidney, and pancreas. They also line the esophagus.
- Cells are also found in ducts and glands, like the bile duct and sailvary glands.
- Epithelia can specialize to act as sensory receptors. They form taste buds, line the nose, and are in the ear. They are also found in the eye.
- Female reproductive organs are lined with ciliated epithelial cells.
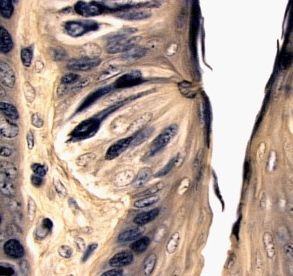
- The skin is made of epithelial cells. Its striated layers demonstrate the extensive morphology of epithelia.
- Capillary beds are made of epithelium.
- Epithelia is the first type of cell to differentiate in the embryo. This occurs during the eight-cell stage.
Functions (not present in every epithelial cell)
| Boundary & Protection | Epithelial cells cover the inner and outer linings of body cavities, such as the stomach and the urinary tract (Figure 3). As the barrier between the outside world’s contaminants and the body, these cells replicate often to replace damaged or dead cells. Many layers provide better protection, meaning if one layer is lost, the underlying tissue is still protected. Tight junctions, are very difficult to alter or break and create a semi-permeable seal that few macromolecules or microbes can penetrate. |
|
| Sensory | Although epithelial cells are avascular, they are innervated. These nerve endings provide signals for sensory sensations such as taste, sight, and smell (Figure 4). These cells exhibit specialized structure to fulfill their function. |
|
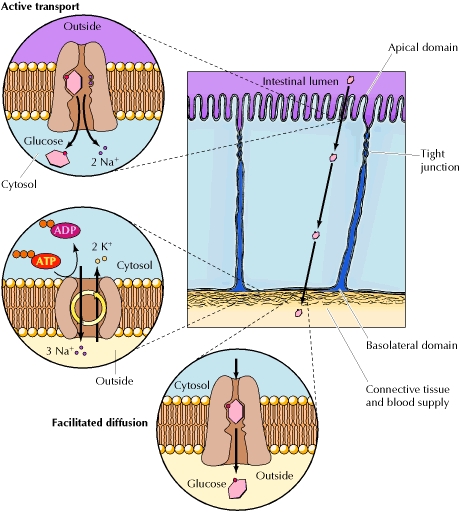
| Transportation | Some epithelial cells, such as the ones found on the intestinal lining, aid in the transportation of filtered material through the use active-transport systems located on the apical side of their plasma membranes. For example, the glucose-Na+ symports located within certain domains of the plasma membrane of epithelial cells lining the intestine enable the cells to generate Na+ concentration gradients across their plasma membranes, which provides the energy needed to uptake glucose, from the lumen of the intestine. The glucose is then released into the underlying connective tissues and is transported into the blood supply through facilitated diffusion down its concentration gradient (Figure 5). |
|
| Absorption | The ability of certain epithelial cells to use active-transport systems, as discussed above, enables them to absorb filtered material, such as glucose from the lumen of the intestine, which can then be circulated to the rest of the body. Cells are also able to endocytose other materials that are necessary for cell growth and signaling. For more information, see transcytosis. |
|
Secretion & Lubrication |
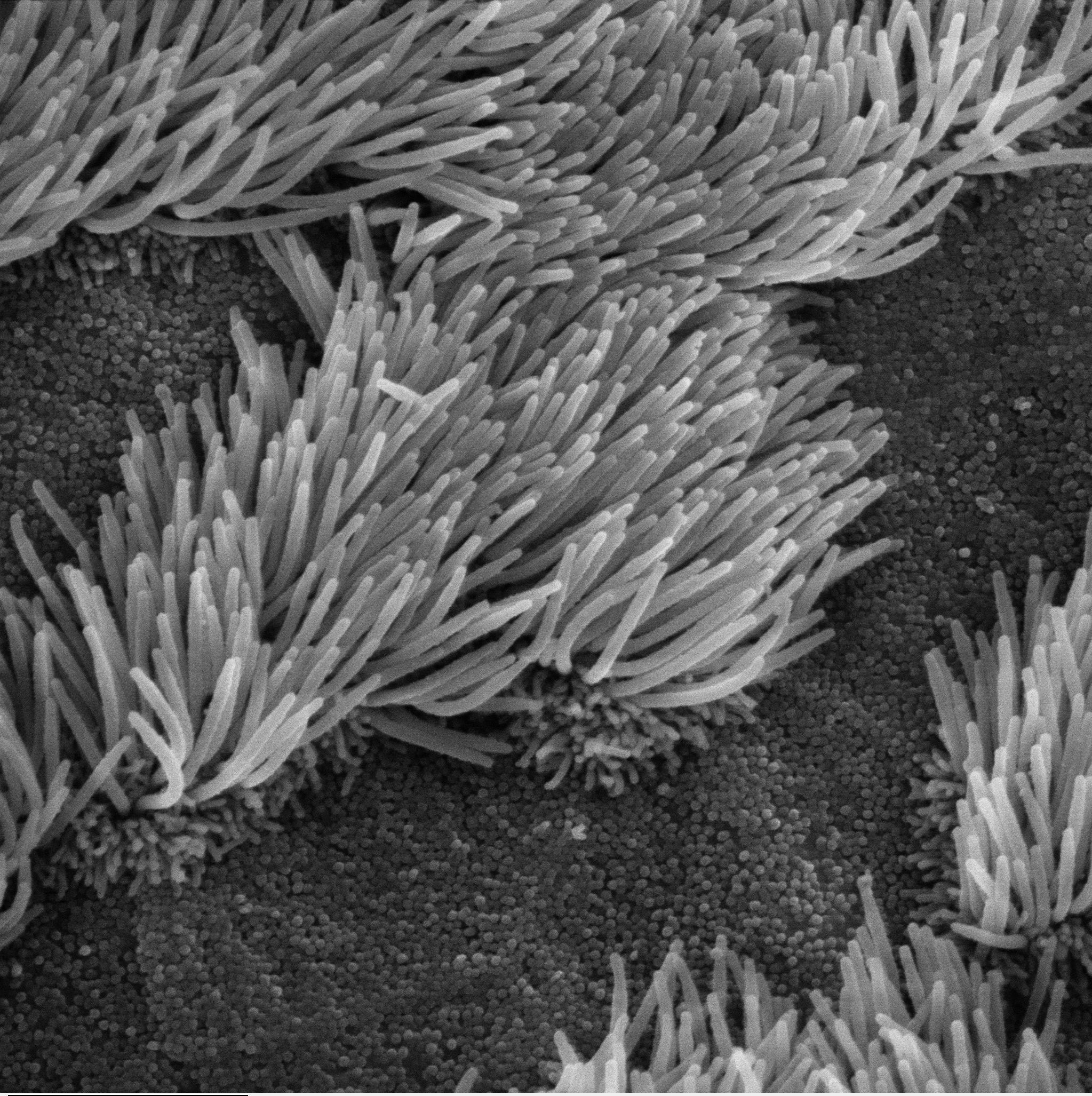
Some epithelial cells, such as the goblet cells, secrete fluids that are necessary for other processes such as digestion, protection, excretion of waste products, lubrication, reproduction, and the regulation of metabolic processes of the body. As part of its excretory role, certain epithelial cells secrete mucus, which lubricate the body cavities (i.e. peritoneum, pericardium, pleura, and tunica vaginalis) and passageways that they line. In the trachea, goblet epithelial cells secrete mucous which provides the lubrication to aid ciliated epithelial cells in sweeping bacteria and dust away from the lungs (Figure 6). In addition, type II alveolar cells excrete pulmonary surfactant, which decreases surface tension, allowing for normal lung function. Figure 6 shows an example of secretory cells in the fallopian tubes. |
|
Movement |
Some epithelial cells have cilia, which aid in moving substances in the lumen by creating a current via coordinated "sweeping" of the cilia (Figure 6). For instance, ciliated columnar epithelial cells are instrumental in the movement of the ovum through the Fallopian tubes to the uterus (Figure 7). |
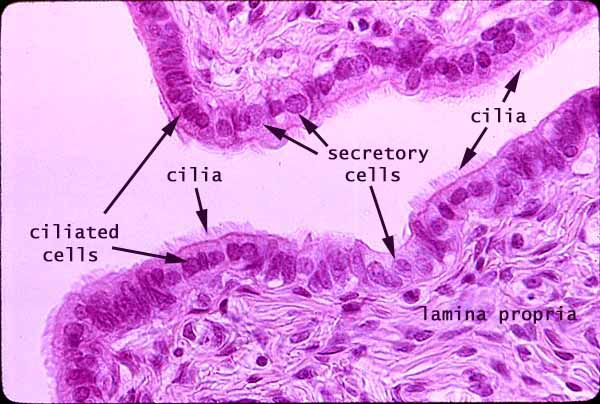 Image from: http://www.siumed.edu/~dking2/index.htm Figure 7. The Fallopian tube is lined with ciliated and secretory epithelial cells. |
Ackerley, S. K. Developmental Biology Online. "Epithelial cells". 09 Dec 2005. 04 Sept 2010
Alberts B., Johnson A., Lewis J., Raff M., Roberts K., & Walter P. (2002). The Molecular Biology of The Cell (4th ed.). New York, NY: Garland Science.
Bezencon, C., le Coutre, J., & Damak, S. (2006). Taste-signaling proteins are coexpressed in solitary intestinal epithelial cells. Chemical Senses, 32 (1), 41.
BIODIDAC - animalia chordata mammalia - L5-8J16.GIF Retrieved 9/8/2010, 2010, from http://biodidac.bio.uottawa.ca/thumbnails/filedet.htm?File_name=L5-8J16&File_type=GIF
Bowen, R. (1998, August 23). Goblet Cells. Retrieved from http://www.vivo.colostate.edu/hbooks/pathphys/misc_topics/goblets.html.
Cooper, G. M. (2000). The Cell, A Molecular Approach (2nd ed.) Sunderland, MA: Sinauer Associates. Reprinted online at: <http://www.ncbi.nlm.nih.gov/bookshelf/br.fcgi?book=cooper>
Curtis, H., & Barnes, N. S. (1989). Biology (5th ed.). New York, NY: Worth Publishers.
Daghlian, D. (2004, April 1). Dartmouth College: Rippel Electron Microscope Facility. Retrieved from http://remf.dartmouth.edu/.
"Epithelium." McGraw-Hill Concise Encyclopedia of Science and Technology. 5th ed. New York: McGraw-Hill Professional, 2005. 839. Gale Virtual Reference Library. Web. 30 Aug. 2010.
Eroschenkodi, V. P. (2005). diFiore's Atlas of Histology with Functional Correlations (10th ed.). Philadelphia, PA: Lippincott Williams and Wilkins.
Gartner, L.P. & Hiatt, J.L. (2007). Color Textbook of Histology (3rd ed.). Philadelphia, PA: Saunders Elsevier.
Gersh, I. (2008). Epithelium. AccessScience. ©McGraw-Hill Companies. Retrieved August 30, 2010 (http://www.accessscience.com/content.aspx?id=YB100222)
Junqueira, & Carneiro. In Basic histology, a text and atlas (11th ed., pp. 299)
King, D.. Histology at SIU SOM. "Epithelium Study Guide". 8 Feb 2010. 5 Sept 2010. <http://www.siumed.edu/~dking2/intro/epith.htm#simpcol>
King, D. (2002, April 5). Fallopian Tube. Retrieved from http://www.siumed.edu/~dking2/erg/oviduct.htm.
http://www.lab.anhb.uwa.edu.au/mb140/corepages/epithelia/images/trachea041he.jpg
Mallery, C. Animal structure and function.http://www.bio.miami.edu/~cmallery/150/physiol/physiology.htm
"Tissue Types Image" 16 May 2007. HowStuffWorks.com. <http://healthguide.howstuffworks.com/tissue-types-picture.htm> 09 September 2010.
Ownby, D. C. The uterine tubes.http://instruction.cvhs.okstate.edu/histology/fr/HiFRp12.htm
Proud, D. (2008). Pulmonary epithelium in health and disease Wiley.
Sadava, D., Heller, H. C., Orians, G. H., Purves, W. K., & Hillis, D. M. (2008). Life: The Science of Biology (8th ed.). U.S.A.: Sinauer Associates, Inc. (Original work published 2006)
Schurch, S., Lee, M., Gehr, P. (1992). Pulmonary surfactant: Surface properties and function of alveolar and airwar surfactant. Pure & Applied Chemistry 64 (11), 1745-1750.