*This web page was produced as an assignment for an undergraduate course at Davidson College.*
Humoral Immune Response
The humoral immune response is critical to long-term HBV clearance (Chang and Lewin, 2007). Acting in conjunction with the cellular arm of the adaptive immune system, the humoral immune response produces antibodies that help control HBV infection. Although both arms of the adaptive immune response aid in clearing infection, neither arm can completely eradicate infection by itself (Bertoletti and Gehring, 2006). Figure 7 below shows an image of a generic antibody structure.
Figure 7. Image from http://www-immuno.path.cam.ac.uk/~immuno/part1/lec06/lec6_97.html
The humoral immune response produces anti-envelope antibodies, which can be detected in human sera following HBV infection. Antibodies to each of the HBV proteins have been detected, although every antibody is not detected in each individual with exposure to HBV (Vranckx, 1983). In fact, the presence of different antibodies indicate different stages of infection. For example, individuals that display anti-HBs (surface antigen) antibodies are thought to have cleared infection, as anti-HBs antibodies are known to contain the spread of infection in the host, remove and destroy viral particles, and prevent reinfection by blocking antigen binding sites on the host’s cells. These are known as neutralizing antibodies and can be found in individuals that have recovered from infection or those that have been vaccinated. Chronic HBV carriers, however, do not have surface proteins. Instead, antibodies to HBV core proteins (anti-HBc) can be detected. Unlike anti-HBs antibodies, anti-HBc antibodies are persistent throughout the course of infection and do not appear to neutralize HBV infection. Additionally, the presence of anti-HBc antibodies do not seem to stimulate the production of anti-HBs antibodies (Huang et. al., 2006). Figure 8 show the presence of these antibodies over the course of infection.
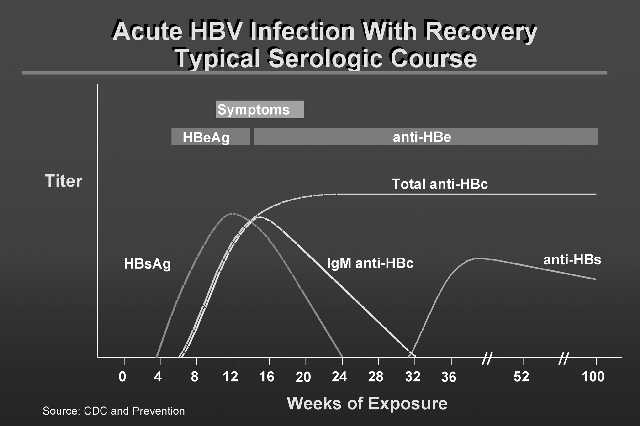
Figure 8. Image from http://www.sin-italy.org/jnonline/Vol15n6/605-f1.jpg
Furthermore, different strains of the hepatitis B virus are composed of different protein combinations, stimulating the generation of different antibody subclasses. More specifically, differences in IgG subclasses in response to antigens correspond to different stages of infection and different types of immune response. For example, individuals with chronic HBV infection exhibit higher concentrations of total IgG and IgG1 than individuals that have recovered from infection. Moreover, chronic carriers exhibit different ratios of different IgG subtypes when compared with vaccinated or recovered individuals. In the case of anti-HBc, chronic carriers demonstrated an anti-HBc IgG subclass pattern of IgG1 > IgG3 > IgG4 whereas recovered individuals displayed a different pattern: IgG3 > IgG1 > IgG4 (Huang et. al., 2006).
Bertoletti, A. & Gehring, A. 2006. The immune response during hepatitis B virus infection. Journal of General Virology 87: 1439-1449.
Chang, J. & Lewin, S. 2007. Immunopathogenesis of hepatitis B virus infection. Immunology and Cell Biology 85:16-23.
Huang, C., Lin, S., Ho, Y., Chen, F., & Yang, C. 2006. The immune response induced by Hepatitis B virus principal antigens. Cellular and Molecular Immunology 3(2): 97-106.
Vranckx, R. 1983. Humoral immune response in Hepatitis B virus infection. Infection 11(2): 114-117.
Return to Christie's Immunology Home Page
Christie Brough. Biology 307: Immunology. Dr. S. Sarafova. Davidson College. May 4, 2007.