*This web page was produced as an assignment for an undergraduate course at Davidson College.*
Evasion of Immune System Detection
Although the mechanism of HBV persistence is not fully understood, researchers speculate that chronic HBV results from multiple factors, including HBV-immune suppression, persistence of stable forms of HBV, and infection of immunologically privileged sites (Chang and Lewin, 2006).
The easiest way to understand immune evasion by HBV is to look at individuals with chronic HBV. Individuals presenting with chronic HBV infection demonstrate diminished CD4+ and CD8+ T-cell responsiveness. It is suspected that low T-cell levels result from high levels of HBeAg, a secretory form of the nucleocapsid antigen, whose function in HBV infection is not well understood. Because HBeAg is not required for viral infection, replication, or assembly, but is still found in all hepadnaviruses, researchers believe that it may have a role in viral persistence (Rehermann and Nascimbeni, 2005). During HBV replication HBeAg is produced in excess and is suspected to have a tolerogenic effect. Often, core-specific T cells are almost undetectable and have a decreased ability to produce IFN-γ. Despite their low responsiveness, CD8+ T-cells are found in the liver where they may cause an inflammatory response but fail to clear the virus (Chang and Lewin, 2006). The figure below shows a microscopic view of HBeAg in hepatocytes.
CD4+ T-cells also demonstrate low levels of response in individuals with chronic HBV. One possible reason for this hyporesponsiveness is an impaired function of dendritic cells. This notion is controversial, however, because the effect of chronic HBV on dendritic cells seems minimal. Another possible cause of this weak HBV-specific T-cell response is the role of regulatory T (Treg) cells, which have demonstrated suppression of immunological responses against self and foreign antigens through specific cytokines and direct cell to cell contact. Studies have shown that depletion of Treg cells in patients with chronic HBV infection have experienced increased function of HBV-specific T-cells. This too is controversial, however, because the same effects were seen in patients with resolved HBV infection (Bertoletti and Gehring, 2006). The figure below shows an scanning electron micrograph image of a Treg cell extracted from a mouse spleen.

Figure 12. Image from http://www3.niaid.nih.gov/NR/rdonlyres/F2974461-0663-479D-91AE-B92ED6E4F6F4/0/hasenkrugFig1.jpg
Other viral factors, such as the HBx protein, may lead to viral persistence of hepatitis B. HBx is known to modify various cellular pathways including NFκB, which may subsequently alter antigen presentation and affect the immune response. Additionally, HBx may upregulate the expression of HLA class 1 molecules on hepatocytes, recruiting T-cells to the liver and causing continued liver damage (Chang and Lewin, 2006).
Another possible mechanism of HBV persistence includes the infection of peripheral tissues that cannot easily be reached by lymphocytes and is ignored by the immune system. Such sites are termed immunologically privileged sites. In such places, viruses can persist without recognition by the immune system. Virions released from these sites, however, can infect liver cells and stimulate memory T-cells, perpetuating liver disease (Chisari and Ferrari, 1995). Finally, epitope mutations facilitate HBV persistence by anergizing B and T-cells rather than stimulating their proliferation (Guidotti and Chisari, 2006). The figure below shows a section of a liver damaged by chronic HBV.
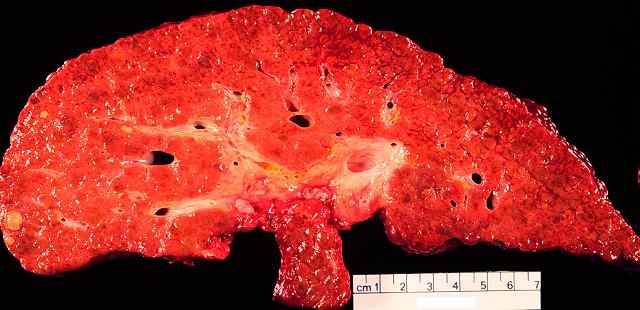
Figure 13. Image from http://www.vaccineinformation.org/photos/hepbuta001.jpg
Bertoletti, A. and Gehring, A.J. 2006. “The immune response during hepatitis B virus infection.” Journal of General Virology 87: 1439-1449.
Chang, J.J. and Lewin, S.R. 2007. “Immunopathogenesis of hepatitis B virus infection.” Immunology and Cell Biology 85: 16-23.
Chisari, F.V. and Ferrari, C. 1995. “Hepatitis B virus immunopathogenesis.” Annual Review of Immunology 13: 29-60.
Guidotti, L.G. and Chisari, F.V. 2006. “Immunobiology and pathogenesis of viral hepatitis.” Annual Review of Pathology 1: 23-61.
Rehermann, B. and Nascimbeni, M. 2005. “Immunology of hepatitis B virus and hepatitis C virus infection.” Immunology 5: 215-229.
Return to Christie's Immunology Home Page
Christie Brough. Biology 307: Immunology. Dr. S. Sarafova. Davidson College. May 4, 2007.