image: T. J. Clark, inc.
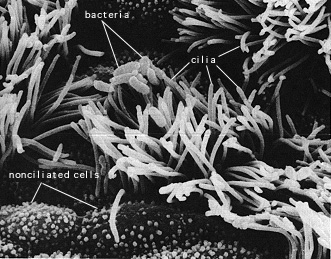
Bordetella pertussis, as a gram-negative bacterium, induces the innate immune response. Two virulence factors, lipopolysaccharide (LPS) and pertussis toxin (PT), act as pathogen-associated molecular patterns (PAMPs) for pattern recognition receptors on macrophages and dendritic cells (Ross et al. 2003). LPS activates macrophages through the Toll-like receptor (TLR) pathway. CD14, acting as the LPS receptor, associates with TLR4 and starts a signaling cascade that leads to NF-kB and AP1 activation in the nucleus (Janeway et al. 2005). These two transcription factors mediate the innate responses to the pathogen. Much of the ability of Bordetella pertussis to colonize and infect human respiratory systems lies in the suppression and evasion of the activation of macrophages and dendritic cells. Interestingly, one study found like TLR4 signaling did not play a critical role in limiting bacterial growth during the first 72 hours of infection (Mann et al. 2005). This indicates that the normal innate response is being significantly altered.
Direct activation of innate immune cells is not the only way that the body can be alerted of the presence of Bordetella pertussis. One study notes that macrophages can engulf pertussis bacteria through “adherence to the CR3 integrin” (Shumilla et al. 2003). CR3 is a complement receptor, so there is indication that a complement response is mounted against Bordetella pertussis.
Activation of the elements of innate immunity has several ramifications. The first of these is the production of cytokines and chemokines. The interleukins (ILs), along with tumor necrosis factor-alpha and chemokines help regulate inflammation, the intensity of immune response, and play a role in activating the adaptive immune response (Janeway et al. 2005). IL-1, IL-6, IL-10, IL-12, IL-23, TNF-alpha, and CCL3 are all known to play a role in pertussis infection (Boyd et al. 2005, Fedele 2005, Ross et al. 2003, Todar 2004). While IL-1, 6, 12, and 23 increase responses such as fever, phagocytic cell recruitment, and vessel permeability; IL-10 suppresses macrophage function (Janeway et al. 2005). Thus, a major strategy of Bordetella pertussis is to alter dendritic cells and macrophages (with virulence factors) to decrease production of cytokines threatening to its survival and increase production of IL-10 (Boyd et al. 2005). Moreover, reducing TNF-alpha and CCL3 production contributes to pertussis survival.
The TLR pathway (when stimulated by LPS binding) also leads to the up-regulation of co-stimulatory molecules on macrophages and dendritic cells (CD80, CD86, CD40, ICAM-1). CD86, CD40, and ICAM-1 are known to play a role in pertussis reactions, as their expression is altered upon pertussis infection (Shumilla et al. 2004). Co-stimulatory proteins are necessary for communication with the adaptive immune system (they activate T cells). Thus, their suppression favors bacterial survival.
Neutrophils are brought to the scene of infection by the recruiting efforts of cytokines and chemokines. Neutrophils usually have the task of controlling bacterial numbers until a full immune response (including adaptive immunity) can be mounted. They accomplish this by phagocytosis, the release of antimicrobial agents, and forming pus. Not surprisingly, Bordetella pertussis has mechanisms to oppose neutrophil function. One virulence factor (adenylate cyclase) can inhibit “chemotaxis, pagocytosis, and superoxide generation” in neutrophils (Boyd et al. 2005).
In a normal innate immune response, particularly one characterized by the release of TNF-alpha, IL-1, and IL-6, edema and fever might be expected. These responses indicate the extravasation of immunological cells from circulation to the site of infection. Moreover, the raised temperature of a fever makes an inhospitable environment to invading pathogens. Pertussis, however, is characterized neither by fever nor by edema (Hoppe 1999). Surely the suppression of the inflammatory response plays a role here, along with the relative localized colonization of Bordetella pertussis.
Bordetella pertussis, although possessing PAMPs that can elicit a full innate immune response against it, has found ways to survive in the human body. The fact that bacteria can be recovered from the body only for the first ten days indicates that the pertussis bacteria capitalizes on its ability to compromise innate immunity until being more successfully attacked by the slower adaptive immunity (bacteria are rarely recovered in the toxemic stage of infection) (Todar 2004). While TLR pathways are activated by LPS recognition, virulence factors such as PT, CyaA, and FHA alter macrophage and dendritic cell function after this activation (Boyd et al 2005, Ross et al. 2004). So, the typical innate response of inflammation, recruitment of neutrophils, phagocytosis, release of cytokines and chemokines, complement activation, and the alerting of adaptive immunity are suppressed. Moreover, parts of the innate immune response are directly blocked. For example, CyaA can lyse eukaryotic cells or inhibit neutrophil function (Boyd et al. 2005). LPS, which can normally be opsonized by the collectin SP-A, is in an altered form. Since SP-A doesn’t bind pertussis LPS, bacterial removal by neutrophils and macrophages (Schaeffer et al. 2004). For more discussion of the way in which Bordetella pertussis avoids the immune response, click here.