This web page was produced as an assignment for an undergraduate course at Davidson College.
This is page 4.
Cellular Immunity of MRSA
Cell-mediated immunity “describes any adaptive immune response in which antigen-specific T cells have the main role. It is defined operationally as all adaptive immunity that cannot be transferred to a naïve recipient with serum antibody” (Immunobiology, 6/e; 2005). T cells serve in the immune response by destroying those pathogens that replicate inside cells where antibodies cannot detect them. Some pathogens can cause infection both in chronic granulomatous disease and in various deficiencies of cellular immunity, and liver infections caused by S. aureus strains are included in this category (http://www.medschool.lsuhsc.edu).
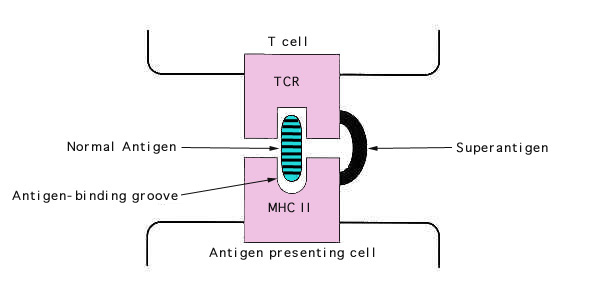
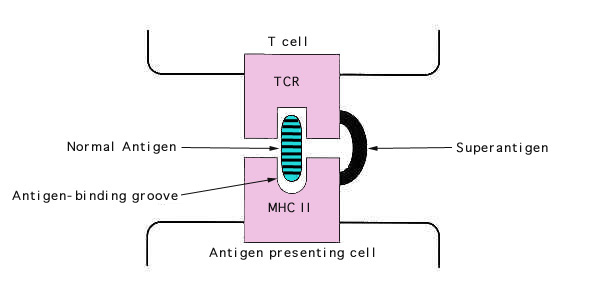
S. aureus secretes two types of toxin with superantigen activity, enterotoxins and toxic shock syndrome toxin (TSST-1). Superantigens stimulate T cells non-specifically without normal antigenic recognition (Figure 4). Up to one in five T cells may be activated, whereas only 1 in 10,000 are stimulated during a usual antigen presentation. Cytokines are released in large amounts, causing the symptoms of TSS. Superantigens bind directly to class II major histocompatibility complexes of antigen-presenting cells outside the conventional antigen-binding grove. This complex recognizes only the Vb element of the T cell receptor. Thus any T cell with the appropriate Vb element can be stimulated, whereas normally, antigen specificity is also required in binding.
© 2005 Kenneth Todar University of Wisconsin-Madison Department of Bacteriology