-
"This web page was produced as an assignment for an undergraduate course at Davidson College."
General Characteristics:
M. tuberculosis is nonmotile and rod shaped (2-4 µm in length and 0.2-0.5µm in width). The generation time of M. tuberculosis is 15-20 hours (Todar 2005). It is an obligate aerobe and requires a host typically for growth and reproduction. Also M. tuberculosis is considered a facultative intracellular parasite that is transferred through the air, which is why tuberculosis appears in the upper lungs first (Quast 2006). M. tuberculosis is gram-positive and nonspore-forming (North 2004).
M. tuberculosis is capable of producing a long term infection which can lead to latent tuberculosis. Immune responses mounted for tuberculosis infections are typically successful at containing, but not eliminating the pathogen (Russell 2007).
.
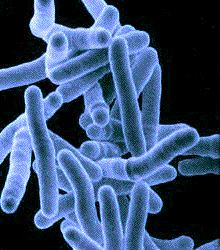
Image of M. tubercuolsis
photo used with permission, www.raw-milk-facts.com
Cell Wall Structure:
The cell wall of M. tuberculosis does contain peptidoglycan and is considered a Gram-positive bacterium although it does not stain as such (Cole 1998). Sixty percent of the cell wall is lipid in particular mycolic acids which are suspected of determining the virulence. Mycolic acids are hydrophobic and help determine the permeability of the cell surface (Todar 2005).
The cell also contains something known as the cord factor. The cord factor is what causes colonies of M. tuberculosis to grow in a serpentine like fashion (Besra 1994).
Reproduction:
Unlike most bacteria, M. tuberculosis can reproduce with in the phagocytic cells of humans including dendritic cells and marophages. In fact, the bacteria will only grow in a warm host (typically human), but can remain alive in a dry start for a few weeks (Brennan 1994). As previously mentioned, M. tuberculosis has a relatively slow generation time of 15- 20 hours (Todar 2005). The bacteria initially grow and divide in the lung alveoli, alveolar ducts, and draining lymph nodes in addition to the phagocytic cells (WHO 2007).
Upon entering a host organism, M. tuberculosis may lie dormant for years or even decades. This may be in part due to the immune response of the host. After the host response dies down, the bacteria remerges and may initiate a full blown infection within the host organism (Cole 1998). M. tuberculosis lives and replicates in the nost cells macrophages and some dendritic cells. The infected macrophages form granulomas consisting of marophages, giant cells, T cells, some B-cells and fibroblasts (Flynn 2001).
Under aerobic condition, M. tuberculosis sustains itself via glycolysis, and oxidative phosphoylation will provide the necessary ATP (Boshoff 2005).
Munoz-Elias (2006) suggests that M. tuberculosis sustains itself on lipids while it replicates within the macrophage endosome. Through the process of B-oxidation, M. tuberculosis degrades and uses host-cell lipids as the precursors for many of its own metabolic processes. M. tuberculosis usually contains examples "every known lipid and polypeptide biosynthetic system" (Cole 1998).
Stages with in Host:
Stage 1: Onset (1-7 days)
Bacteria is inhaled through the air and typically engulfed by alveolar macrophages. At this instant, disease progression depends on the virulence of the inhaled strain and the antimycobacterial capabilities of the macrophage in question. In some cases, the bacteria are able to reproduce and initiate the infection (Dannenberg 1994). Tuberculosis begins when the inhaled mycobacterial muclei reach aveolar machrophages (Todar 2005).
Stage 2: Symbiosis (7-21 days)
If the initial macrophage does not succeed in killing the bacteria, the bacteria will replicate until the macrophage bursts. The bacteria are now engulfed by other alveolar macrophages and nonactivated macrophages. The macrophages that arrive from the bloodstream engulf the exposed bacteria in a symbiotic manner—neither the host nor the bacteria is harmed (Danenberg 1994).
Stage 3: Initial Caseous Necrosis (14-21 days)
The next stage of disease development begins when bacterial reproduction slows. Growth slows because as the bacteria reproduce, they kill all the surrounding nonactivated macrophages and run out of cells to divide within. In addition, the increased number of bacteria produces anoxic conditions and reduces the local pH (Dannenberg 1994). The bacteria can no longer reproduce in this tubercule, but can remain alive for long periods of time at this state. Tubercules are also described as caseous centers due to their appearance (Todar 2005). The host kills its own tissues to prevent the spread of the bacteria. Also at this stage, the host will test positive for tuberculin (Dannenberg 1994).
As the granulomas mature, they show more vacularization and develop a capsule which somewhat separated macrophages, granulocytes, and the lympocytic infiltrate. As the disease contiunes to progess, the center of the granulomas lose vascularization and undergo necrosis (hence the name caseaous necrosis) (Russell 2007).
Also at this stage, T-cells begin to recognize presented M. tuberculosis, which causes T-cell activation and production of cytokines inlcuding INF-gamma. INF-gamma activated that macrophages, increasing there ability to destroy the invading bacteria (Todar 2005).
Stage 4: Interplay of Tissue-Damaging and Macrophage Activating Immune Response (After 21 days)
Macrohpages surround the tubercule, some of which may be inactivate. M. tuberculosis uses the inactive macrophages to reproduce, causing the tubercule to grow. The tubercule may break off or spread into the bronchus, and then other parts of the lung. If the tubercules reach the blood stream, the patient can develop tuberculosis outside of the lungs, which is known as milliary tuberculosis. Secondary lesion can develop almost anywhere within the body, but are commonly found in the bones, joints, lymph nodes, and genitourinary system (Todar 2005).
Stage 5: Liquification and Cavity Formation
At some point the centers of the tubercules may liquify, which produces a very conducive enviornment for the bacteria and rapid spread of the disease. Only a very small precentage of infected individuals will progress to this stage (Todar 2005). The following picture is an example of what cavity formation looks like in the lungs.
Reactivation—Latent
Remergence of TB after the primary infection maybe triggered by various factors including HIV/AIDS, poor nutrition, old age, and stress (Russell 2007).
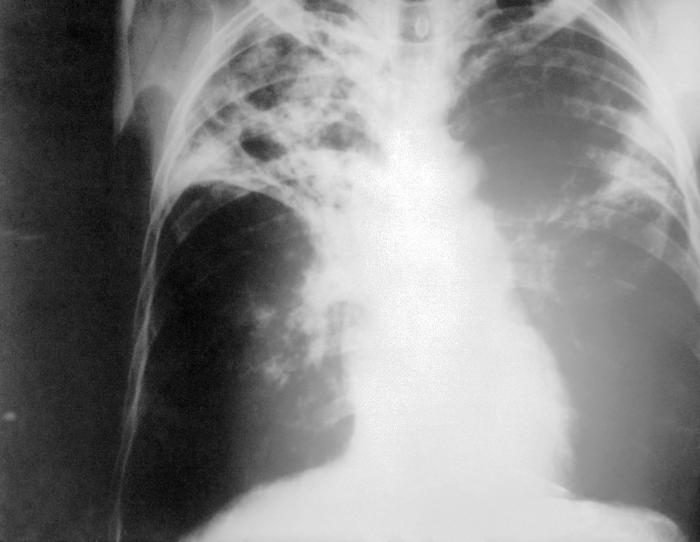
X-Ray image of patient's lungs with M. tuberculosis infection from CDC website
This site was created as partial fulfillment of requirments for Biology 307 at Davidson College in the Spring Semster of 2007.
Davidson Home Davidson Biology Home
Questions and comments should be directed to Dr.Sarafova or to the site creator Emily Rivard