Treatment and Future Directions
Diphtheria was first described as a clinical disease in ancient Greece, Syria and Egypt as early as the 4th century B.C. Epidemics of clinical diphtheria have been recurring since then until modern times across the world. In 1884, Friedrich Loeffler was the first to identify C. diphtheriae as disease causing agent in diphtheria. He also discovered the soluble exotoxin that causes the clinical disease. In 1900, Emil von Behring and Kitasato Shibasaburo made the earliest attempts to induce immunity against diphtheria were performed on guinea pigs. They successfully immunized guinea pigs using a heat-attenuated form of the toxin. They also discovered that serum from immunized guinea pigs could be used to protect other animals, but unfortunately not humans, against the disease. In 1909, Theobald Smith devised the first vaccine against diphtheria for humans. This vaccine consisted of toxin neutralized by antitoxin produced by horses. However, this vaccine was extremely toxic and allergenic in humans and was only used for a short time. Finally, in 1929 Gaston Ramon discovered that diphtheria toxin loses its toxigenic properties but retains its antigenic properties when treated with formaldehyde and heat. Toxin that has been deactivated by treatment with formaldehyde is called toxoid. The use of toxoid as a diphtheria vaccine quickly became widespread and is still in use today. The modern toxoid vaccine usually is administered in a combined vaccine that also protects against tetanus and pertussis, commonly referred to as DTP. The toxin used to make the vaccine is isolated from the PW8 C. diphtheriae strain, which produces an unusually large amount of the toxin (Holmes, 2000; Todar, 2002).
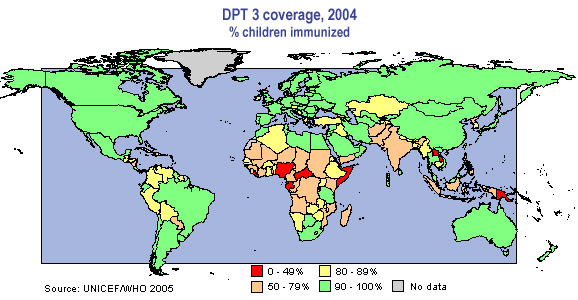
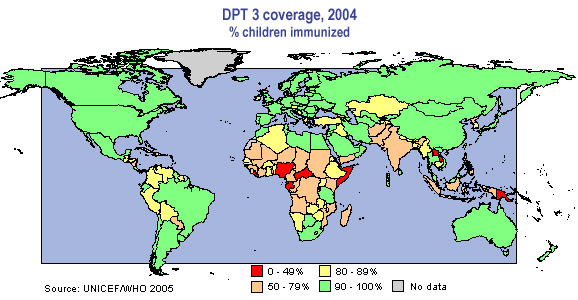
http://www.childinfo.org/areas/immunization/status.php
There seems to be no clearly defined level of circulating anti-toxin antibody that gives complete protection against diphtheria. To be a symptom-free carrier of the bacteria an individual must have an antibody level above 0.16 IU/ml, while a level of 0.01 IU/ml provides some clinical immunity. Immunity seems to degenerate after a period of time. In other words, to maintain an protective level of antibodies in circulation, an individual must be re-exposed to the toxin periodically. The initial vaccination and re-exposure can occur through administered vaccinations or through passive immunity and subsequent natural exposure to the bacteria. Passive immunity occurs in infants who gain immunity from their mothers during gestation. During the pre-vaccine era in the United States, most infants were born with passive immunity and natural immunity developed in most individuals through subsequent exposures to diphtheria in the environment. This pattern of acquiring natural immunity is seen in modern developing countries without widespread vaccination. Developing countries are especially at risk to diphtheria epidemics. The high level of risk is due to the lack of widespread vaccination and the high incidence of skin infections which create a reservoir for diphtheria colonies. Mass immunization has been shown to significantly reduce the occurrence of clinical diphtheria, however it is essential that immunity is kept at effective levels either through booster shots or natural exposure to the toxin (Galazka, 1996). In the United States, diphtheria has nearly been eradicated. From 1971-1981 in the United States, 1288 cases of diphtheria were reported mostly among populations in poor socioeconomic conditions. Between 1980 and 1994, the number of reported cases had dropped to 41 (Bisgard et al., 1998).
Vaccination only protects against the toxin itself, not against the initial infection by C. diphtheriae (Chen et al., 1985). To treat the clinical disease, antibiotics such as erythromycin or procaine penicillin G are administered orally or by injection. Antitoxin produced from horses is administered to stop the spread of the disease. Antitoxin is ineffective against toxin that has already bound or entered a cell, but it will neutralize unbound, circulating toxin. A patient is usually no longer contagious after taking antibiotics for 48 hours (Centers for Disease Control and Prevention, 2007).
References
Bisgard, Kristine M., Iain R. B. Hardy, Tanja Popovic, Peter M. Strebel, Melinda Wharton, Robert T. Chen and Stephen C. Hadler. "Respiratory Diphtheria in the United States, 1980 through 1995." American Journal of Public Health 88.5 (1998): 787-791.
Centers for Disease Control and Prevention. Epidemiology and Prevention of Vaccine-Preventable Diseases. Atkinson W, Hamborsky J, McIntyre L, Wolfe S, eds. 10th ed. Washington DC: Public Health Foundation, 2007.
Chen, Robert T., Claire V. Broome, Robert A. Weinstein, Robert Weaver, Theodore F. Tsai. "Diphtheria in the United States, 1971-1981." American Journal of Public Health 75.12 (1985): 1393-1397.
Galazka, Artur M. "Module 2: Diphtheria." The Immunological Basis for Immunization Series. Geneva: World Health Organization, 1996.
Holmes, Randall K. “Biology and Molecular Epidemiology of Diphtheria Toxin and the tox Gene.” The Journal of Infectious Diseases 181 (Suppl 1) (2000): S156-67.
Todar, Kenneth. Diphtheria. 2002. <http://textbookofbacteriology.net/diphtheria.html> Accessed 4 Feb 2007.